CALIFORNIA, USA — This story was originally published by CalMatters.
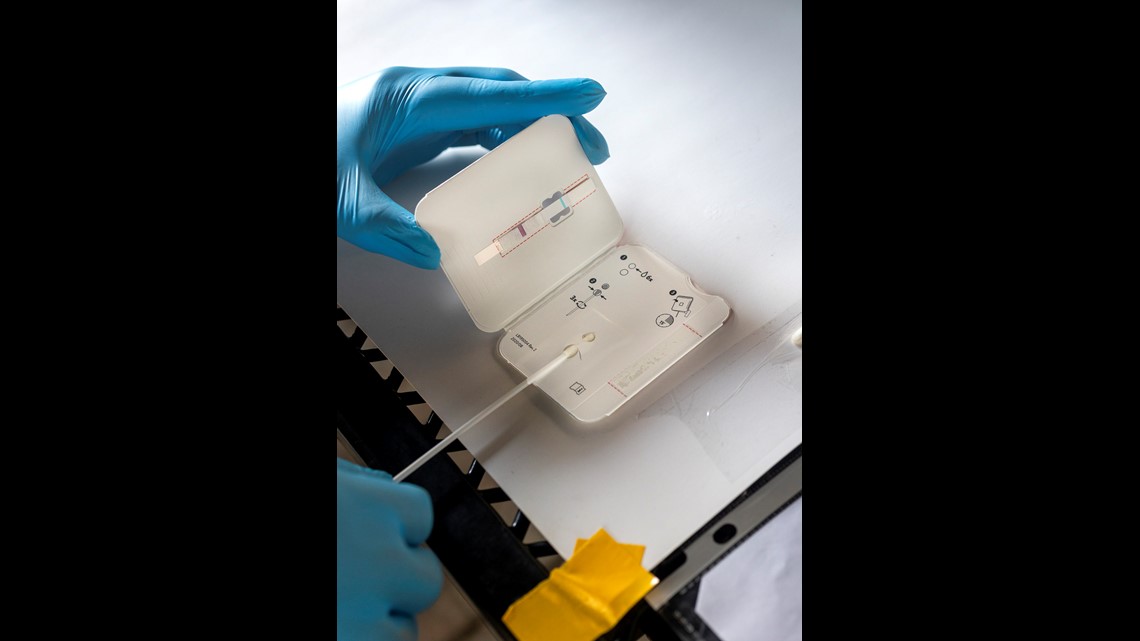
Sarah Voit likes to keep 10 to 15 rapid test kits on hand in case any of the residents of the Family Emergency Shelter Coalition in Hayward need to be tested for COVID-19. They’ve had some infection scares, and the antigen tests — which return results in minutes — have been crucial to curbing the virus in the family shelter.
But in recent weeks, the staff has struggled to purchase enough rapid test kits. The local Walgreens and Costco have started limiting sales to one per customer. “We ran into the same issue at the beginning of the pandemic when we were trying to buy Clorox wipes and hand sanitizer,” said Voit, the shelter’s program director.
Three weeks ago, a child living at the shelter was sent home from school after a classmate contracted COVID-19. Voit’s team used the rapid tests on the whole family. They all came back positive.
“Because we had those kits on hand, we were able to send them immediately to the isolation and quarantine hotel the county runs,” she said. “Otherwise it could have taken three to five days to get those results and many more families could have gotten sick.”
A nearby clinic offers COVID-19 tests, but only PCR tests, which usually take several days for results. Even a single day’s wait could fuel an outbreak among the shelter’s 23 adults and children.
“If a resident really needs a test, we can send them there,” Voit said, “but the three to five days is tough to wait.”
Voit managed to find an online supplier and ordered 70 kits for the shelter, but they aren’t coming anytime soon: The delivery date is a month out.
Online and in stores, major retailers are sold out of the popular at-home tests, and medical supply vendors can’t find enough rapid test kits for schools, shelters, nursing homes, employers and other groups. Across the state, people in low-income communities are being turned away as community groups and clinics are forced to ration their tests. Workers in need of regular screening for employment struggle to find them. Some parents are spending hundreds of dollars out-of-pocket to test their school kids. And nursing homes are told they may have to wait weeks for testing kits.
“The U.S. gets a D- when it comes to testing,” said Dr. John Swartzberg, an infectious disease expert and professor emeritus at UC Berkeley. “We’re not doing enough of it and it’s too difficult for people to get tests. Those with the least resources have the greatest difficulty in finding a free test site or purchasing at-home testing.”
Experts say quick and easy testing is vital to contain the spread of COVID-19. Without widespread access to tests, people don’t know they are infected and need to quarantine, causing outbreaks that could have been prevented.
“There should be little stations where you can get rapid tests anywhere, anytime,” said Joe DeRisi, professor of biochemistry and biophysics at UC San Francisco.
Rapid test kit shortages abound
It’s a mismatch of supply and demand. Although the state is reporting record-high testing numbers, Californians seeking same-day results and over-the-counter test kits for sniffling kids, employer verification, or merely peace of mind say they are unavailable. The problem: Nearly all state-run testing facilities offer only laboratory-based PCR tests, and people want rapid ones instead.
When the Delta variant reared its head, the shortage of rapid tests created the “perfect storm,” experts say. The surge coincided with schools reopening and employers requiring quick, routine testing. At the same time, local health departments scaled back their testing efforts, focusing on vaccinations instead. Manufacturers, seeing decreased summer demand, reportedly shuttered production lines and tossed unsold product.
Fewer than 10% of testing locations across the state now offer rapid-result antigen tests, according to a database from Coders Against COVID and URISA GISCorps.
The test shortage is so severe that the federal government has stepped in to increase production. On Sept. 9, the Biden Administration announced a national COVID-19 action plan that includes the purchase of 280 million rapid point-of-care and over-the-counter tests by the federal government and a three-month deal with Walmart, Amazon and Kroger to sell the tests at cost.
The U.S. Department of Health and Human Services did not respond to requests inquiring how many rapid tests would be allocated to California.
Industry experts say manufacturers, including Abbott Laboratories, are picking up production, but adequate supplies have yet to hit the shelves for consumers — and it could be weeks off.
“We have been told by this particular manufacturer that they’ve caught up, but clearly at the customer level we still see shortages, and of course customers are shifting to other brands which cascade the shortage elsewhere,” said Nam Tran, professor of clinical pathology at UC Davis and a member of the state’s COVID-19 Testing Task Force.
Despite the slightly lower sensitivity of rapid tests compared to laboratory-based PCR ones, the ease of the at-home options make them ideal for community surveillance, DeRisi said. PCR tests can detect lower levels of virus and potentially catch an infection sooner, but the reality is the inconvenience of scheduling an appointment means people aren’t getting tested enough.
“I could get a PCR, but that’s just a snapshot in time,” Tran said. “If you want people to test every day, (PCR) is not feasible.”
About 90% of all PCR test results are returned in two days, according to state data, although that time has steadily crept upward recently. The 15 minutes of wait for a home rapid test compared to 48 hours could mean the difference between an infectious person starting quarantine immediately versus spreading the virus for several days.
And it’s clear that rapid testing works.
The Mariposa skilled nursing facility that Katrina Anderson manages hasn’t had a single case of COVID-19 among its frail residents since the beginning of the pandemic.
In addition to other strict infection control policies, every person that enters the building is given a rapid test.
“If you come to work in our facility you’re tested. If you come to fix something that’s broken in the facility, you’re tested,” Anderson said. “Nobody enters without getting a rapid test.”
Anderson received word from the state that tests were in short supply. She was able to secure enough kits for the next few weeks. But other organizations, like schools and community groups, attempting to set up rapid testing through the California Department of Public Healthmay not be so lucky. The Testing Task Force website warns that it will take six to eight weeks to receive the state’s rapid test kits.
Schools desperate for test supplies
In March, the state offered 5 million BinaxNOW tests to schools as an optional incentive to reopen in the spring.
Rapid testing is a major strategy for schools eager to avoid kids’ time spent out of the classroom sick or in quarantine. But the state program has been swamped with orders, and some schools say PCR testing is their only reliable option right now.
State public health officials told Kern High School District in Bakersfield “that there is a nationwide shortage of antigen/rapid tests,” said Erin Briscoe-Clarke, a district spokesperson. So the school is using PCR tests instead despite the longer wait time for results.
DeRisi from UCSF said he heard that “hundreds of schools” signed up in September for the state tests, “right when the shortage occurred and right when the Delta bump hit.”
The state Department of Public Health did not return requests for comment about its ability to fill schools’ orders.


Officials at the Clovis Unified School District northeast of Fresno said they have struggled to secure enough rapid tests for their 43,000 students. In addition to required masking and daily health screenings, the schools there routinely test students involved in extracurricular activities and are gearing up to begin testing faculty weekly. The schools also shorten the 10-day quarantine period by three days if a student can prove they are COVID-negative.
But the Clovis district was notified earlier this month that the state may not be able to fill its test kit order, spokesperson Kelly Avants said. “We got our order in and heard within a day or two that the state was no longer accepting additional orders because they were out,” Avants said.
Early this month, the Clovis district contacted more than 40 vendors in search of rapid test kits. Nobody had any in stock and wouldn’t until at least October, maybe even December. Eventually, the state was able to fulfill the district’s order.
“Like so many other supply chains right now, it is unpredictable,” Avants said.
The district has about a two-week supply of tests, and expects a delivery of 12,800 more from a private vendor soon.
Without rapid testing readily available publicly, some parents are spending hundreds of dollars to monitor their kids’ health.
Nayamin Martinez, a parent in Clovis Unified, received an email several weeks ago that a child in her daughter’s classroom tested positive for COVID-19.
It was a Friday afternoon, and the family’s local Kaiser testing clinic was closed. Even with insurance, Martinez couldn’t find a rapid test kit or same-day appointment anywhere. She also knew that results from a PCR test wouldn’t come until the following Monday or Tuesday and didn’t want to keep her daughter out of school needlessly.
Martinez wound up taking her to urgent care and paying $270 for the rapid test — and her peace of mind.
Hundreds of testing sites shut down
The California Department of Public Health says there’s a glut of PCR testing capacity. Thousands of same-day appointments for the tests are available through the state testing website, and more tests are processed daily now than during the winter surge. OptumServe, which manages the state’s testing efforts, works with the state to monitor demand and offer drive-thru, mobile and fixed site options, health officials told CalMatters.
Yet many Californians complain that they can’t find an appointment or a rapid test. The issue: As government-run mass testing sites have closed, it’s not always clear to people where new locations have sprung up.
“You end up with barriers to access that have less to do with capacity and more to do with lack of information,” said Dr. Jorge Caballeros, a physician and founder of Coders Against COVID, a volunteer group that crowdsources a directory of test sites nationally.
“More of the testing has shifted from a government-based or public health service and become privatized. A lot has shifted to primary care physicians, health systems and to companies that are running these tests,” he said.
According to the Coders Against COVID database, 900 testing sites have closed in California since April 2020, and that’s likely an undercount.

Working-class and immigrant communities that often face technological or language barriers are struggling with the shifting test locations and longer turnaround times. Community organizations have been left to fill the gaps with what little supplies they have left.
“We’re still the only organization in Marin County that’s doing rapid testing for free, and I don’t understand why,” said Yolanda Oviedo, COVID-19 response manager at Canal Alliance. “It’s been really hard for us to maintain.”
Canal Alliance, which provides an array of services for the Latino community in Marin, offers rapid testing two days a week.
The pandemic hit the county’s Latino population hard. Latinos accounted for 80% of the county’s COVID-19 cases last year despite making up less than 16% of the population. Most are essential workers with high risks of exposure.
Oviedo said the group received 5,000 test kits from the state in May and have used more than 3,000. Demand has grown since August, and they have resorted to limiting testing to 100 people per day in order to make supplies last as long as possible.
People seeking tests at the site are frequently turned away. It’s a tough decision, especially when they know community members are desperate, said Marina Palma, San Rafael City Schools board member and volunteer at Canal Alliance.
“We have people coming to test with us from Richmond, Petaluma, Novato, San Francisco,” Palma said.
Increasingly employers, like Amtrak and Goldman Sachs, are requiring proof of vaccination or negative test results, and many workers can’t afford to miss a day of work.
“When you go to other places, it takes two days for the results. Two days means a lot for those families who work labor,” Palma said. “If they don’t have that verification, they can’t support their families.”
It’s a similar story in the Central Valley, where Martinez, the Clovis parent, is the executive director of the Central California Environmental Justice Network. Her organization, which partnered with UC Davis, is the only place in Yolo, Stanislaus, Madera and Fresno counties offering rapid tests.
Several weeks ago they, too, started capping the tests at 100 per day.
“When I heard we were capping (tests), I asked ‘Why don’t you order more?’ They said ‘There’s no more to order. They’re on backlog,’” Martinez said.
Many of the people they test have Medi-Cal or are uninsured, and are unable to get appointments at local health clinics. Routine testing for employers isn’t necessarily covered by insurance.
Everyday around 5 a.m., people start calling Martinez, desperately searching for a free test. “It’s bureaucracies after bureaucracies. It’s exhausting,” she said.



