SACRAMENTO, Calif — For the past five weeks, Chad Baker has called his hotel room home. The Emergency Room Nurse at Kaiser Permanente Richmond has been living in the hotel to protect his husband of six years from contracting the coronavirus.
As a healthcare worker on the front lines of the coronavirus pandemic in California, Baker knows all too well the dangers of coming home after his shifts. If he brings the virus home to his husband who already suffers from respiratory issues, it could be deadly.
"You know, he's my rock and the center of my world, and to be separated from him is heartbreaking,” Baker said.
The work is dire for California healthcare workers, of whom at least 1,803 have tested positive for COVID-19 on the job, by community spread, or by travel. That’s the stress that Baker walks into the hospital.
On top of that, the Bay Area couple has financial anxiety, having to dip into their savings to pay for the room. The hotel serves as a safe place for Baker to rest his head for a couple hours before working 8, 12 or 16 hour shifts at Kaiser Permanente Richmond.
But it’s also akin to “having more than one mortgage,” Baker said.
But the alternative is too risky.
It’s a story familiar to many healthcare workers across the state who have decided to not take any chances putting their family’s lives on the line — opting instead to pay out-of-pocket to stay in hotels or even sleep in their cars.
"This simply isn't acceptable," Gov. Gavin Newsom said Thursday during a press conference announcing a plan that would give a reprieve to those same healthcare workers.
The new initiative would provide free or low-cost hotel rooms to healthcare workers who have been exposed to, or tested positive for, the coronavirus. For low-wage workers, expenses could be 100% reimbursed. (Click here for more)
“California is fighting to protect those who are protecting us,” Newsom said. “Health care workers are the heroes of this moment. As we ramp up the workforce to meet the demand we are also stepping up to help keep our workers’ families safe by providing hotels as temporary housing options.”
So far, the state has secured 150 hotel rooms near hospitals in priority counties including Contra Costa where Kaiser Richmond is located, the hospital in which Baker works.
"So more care, for our heroes, for our caregivers at a time when we need to be there for them,” Baker said.
Baker said the health care system has failed its workers in the face of the pandemic, and he doesn't know how long he could sustain the current hotel room he's in.
"Our healthcare systems have to support us, and I'm glad that governor newsom is stepping up and trying to do that,” Baker said.
California steps up
The initiative is just one of several unveiled in recent weeks by Newsom that would help the thousands of California healthcare workers who have worked to save the more than 18,300 people who have tested positive for COVID-19 across the state.
At the end of March, Newsom launched an initiative to expand California’s health care workforce and recruit health care professionals ahead of the expected surge. The initiative called of retired nurses, nursing students, healthcare professionals with an active license, and more to join the California Health Corps.
On Monday, Newsom announced that the state was changing the Sacramento Kings old home, the Sleep Train Arena, into a makeshift hospital for COVID-19 patients. It's part of an attempt to add 50,000 hospital beds to the state's existing hospital capacity of nearly 75,000 beds.
Then, on Wednesday, Newsom said that he procured a monthly shipment of 200 million N95 and medical masks for healthcare workers. The announcement comes as states in America have largely had to turn to the open market to get masks and other supplies, or even compete with other states and the federal government for personal protective equipment.
"In an effort not to play small ball, in an effort to really organize, to meet the audacious goal that we have of over 500 million PPE… we decided to retool our efforts, refocus on our vendors, refocus on our supply chain," Newsom said.
California lawmakers are pressing Newsom's administration for more details on how it will distribute and ensure the quality of hundreds of millions of new protective masks it's buying amid the coronavirus outbreak.
State Sen. Holly Mitchell asked Newsom's finance director Thursday for details on the contract Newsom announced to bring 200 million masks per month into the state. Her request came in a letter allowing Newsom to spend money to execute the contract quickly.
But Mitchell says lawmakers need more detailed information on who will get the masks.
Bracing for the peak
Still, the PPE will come to California hospitals just in time as models show California’s peak of coronavirus cases is coming soon.
More than 18,300 people have tested positive for the coronavirus in California, and 492 people have died. That, despite having taken several aggressive measures like social distancing and stay home orders to mitigate the spread of the virus across the state.
But according to the Institute for Health Metrics and Evaluation, that will become worse very soon as the peak in California is estimated to be around April 14. Peaking is an estimation between the number of people infected with COVID-19, the medical resources available and deaths.
While the IHME and University of Washington’s model predicts April 14 for all of California, counties differ on a case-by-case basis.
During a press conference Saturday, Newsom acknowledged national models that show April as the peak. But he said models from his office show a peak in the first few weeks of May.
READ MORE:
"Our modeling is not done in isolation. It’s done in collaboration... with the systems, the health care professionals. It’s done by taking a look at everyone else’s modeling and incorporating some inputs on the basis of expectations and we recalibrate ours," Newsom said.
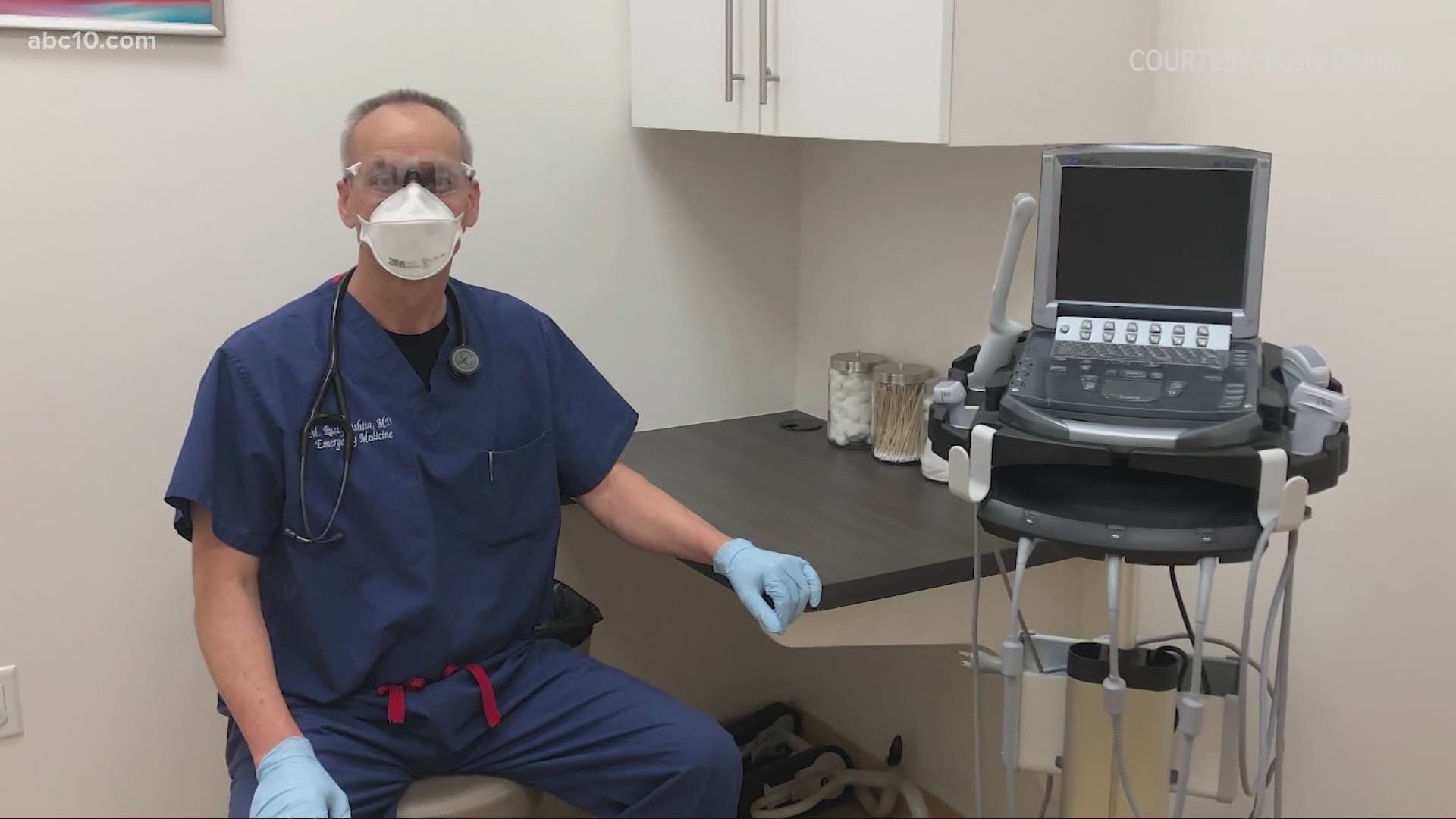
Regardless of the expected peak, California healthcare workers like Dr. Rusty Oshita are ready for what’s to come.
Dr. Oshita, an emergency physician for the Northbay Medical Center in Fairfield, was in the middle of planning a trip to take around 10 other doctors, nurses and other healthcare workers to help with overflowing hospitals in New York where more than 151,000 people have tested positive and more than 7,000 people have died from COVID-19.
Dr. Oshita, whose two urgent care facilities in Sacramento recently started offering coronavirus testing, said the group was going to fly across the country to the patients in the state as well as “the healthcare providers that have been working so tirelessly.
That was up until a few days ago when new models were released predicting California's peak could actually be coming on April 13 — one day before the group was supposed to leave. The group decided it was best to stay and help the possible surge coming to their home state next week.
“It's time to strike back. It's time to start knocking this COVIS-19 down,” Dr. Oshita said. “It's time to get rid of this thing. It really is time to kick that COVID-19 butt and get on with our American way.”
Whether California can stand strong during the coming surge is to be determined. The state did see good news on Thursday, ahead of the expected peak as California saw its first daily decrease in intensive care hospitalizations during the coronavirus outbreak.
Newsom said Thursday the number of ICU placements declined by 1.9% on Wednesday. He said the decline was encouraging, but urged people not to read too much into it.
Newsom has said the number of ICU hospitalizations is a key indicator for how many health care workers and medical supplies the state needs.
Newsom also said California hospitals are using only about one-third of their ventilators. He said about 8,000 ventilators are available.
From California to New York
Not all California healthcare workers will be in the state to help if the surge comes.
Ann Nichols, a retired nurse from Sacramento, is spending weeks working at a makeshift overflow hospital in Central Park in New York City. Nichols is part volunteering her time working on the front lines of the coronavirus pandemic with a team from Samaritan's Purse.
Nichols said she’s done three Disaster Aid Response Team missions now. The days are long — often 14-hours — and the amount of patients they treat in New York City is daunting.
“It’s rough. I'm not going to lie. It's hard,” Nichols said. “My body tells me these are long days on my feet, but when I look at the suffering going on with my patients, I have nothing to complain about.”
In a Skype interview, Nichols walked ABC10 around the makeshift hospital near Mt. Sinai Hospital in Manhattan where they get their patients from. Tents are set up for men and women to change into their PPE and for them to take off their protective gear to avoid contamination.
READ MORE:
Nichols said the patients are in what’s called the “hot zone.”
“Behind the gates and fences — it's all gated off,” Nichols said. “We are using Ebola precautions. We don't want anything going in to come out. Anything going in cannot come out.”
Nichols said, no matter the patient, she's been praying with each and every one.
She has dedicated four weeks to this mission but said she realizes she may have to extend her time in New York based on the sheer number of people testing positive for the virus daily.
“I'm still hearing this is like the flu. This is no the flu. This is a terrible disease,” Nichols said. “I'm hoping people are taking it seriously. Stay home. If you stay home you can't get the disease.”
FOR THE LATEST CORONAVIRUS NEWS,
DOWNLOAD THE ABC10 APP:
►Stay In the Know! Sign up now for ABC10's Daily Blend Newsletter